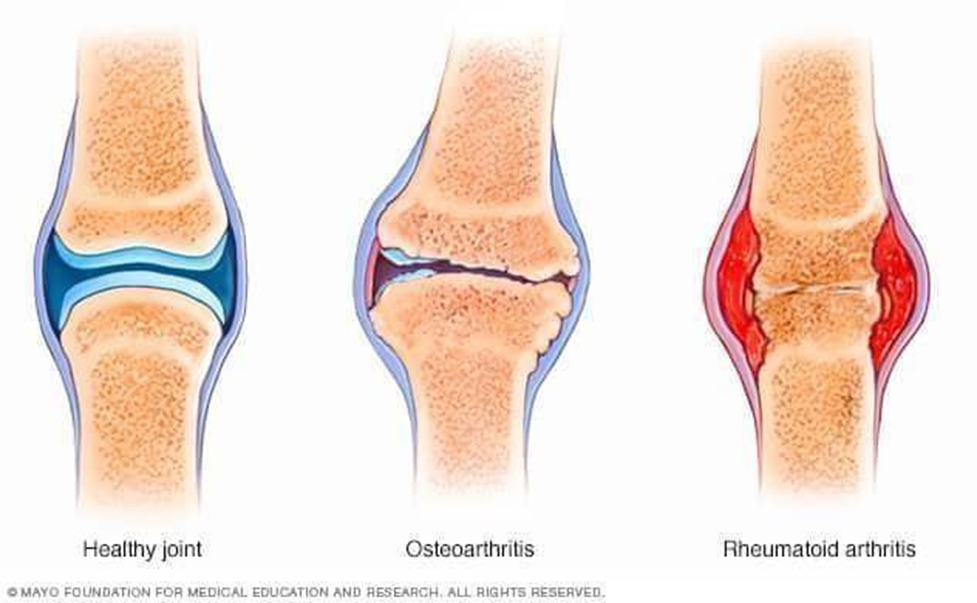
Arthritis means inflammation or swelling of one or more joints. It describes more than 100 conditions that affect the joints, tissues around the joint, and other connective tissues. Specific symptoms vary depending on the type of arthritis but usually include joint pain and stiffness.
ETIOLOGY:
1. Hematogenic spread of infectious agents arising from generalized septicemia or localized suppurative process elsewhere in the body, reaching the joints). Arthritis may develop secondary to mastitis, metritis, endocarditis, suppurative pneumonia, pyelonephritis, and other septicemic conditions. Arthritis may also develop from extension infection from local skin lesions.
The common bacteria isolated from arthritis in animals are Streptococcus spp., E. coli, Corynebacterium pyogenes, Chaetophorous necrophobic, Staphylococcus spp., Actinobacillus equuli, Salmonella: spp., Chlamydia psittacosis, and Mycoplasma spp.
2. Specific diseases; Arthritis may also develop as an associated lesion of some specific diseases, including tick pyemia of lambs, tuberculosis, strangles, Mycoplasma mycoides sp• mycoides infection (goats); serositis arthritis in sheep and goats, caprine arthritis encephalitis virus infection, brucellosis, bovine viral diarrhea, and. Ephemeral fever.
PATHOGENESIS:
The exact mechanism of arthroplasty development is not well understood. Primary arthropathy is a part of normal aging processes and ordinary joint usage. With increasing age, there is a loss of normal resilience of cartilage, because of the lowering of chondroitin sulfate and reduction in permeability of the cartilaginous matrix, which can result in progressive degeneration of articular cartilage.
CLINICAL PATHOLOGY:
Aspiration of joint fluid with a sterile needle may be obtained for its biochemical and cultural examinations. Blood examination may reveal! leukocytic changes (and left shift), depending upon the severity of the infection. X-ray examination may be helpful, particularly in chronic cases, to identify the severity of lesion development at the articular surface and adjacent bones. Serological tests may assist in the diagnosis of specific.
NECROPSY FINDINGS:
Varying in the degree of pathological lesions depends upon the severity and duration of the disease. A thickening and roughening of a synovial membrane, erosions at articular cartilage, and the presence of fiorino-purulent exudate are suggestive of acute arthritis. Chronic arthritis is characterized by ossification at articular cartilage and surrounding surfaces. The synovial fluid is changed both in quality and quantity and may contain the causative bacteria.
Characteristics of synovial fluid:
Normal Suppurative arthritis Degenerative arthropathy* Color Clear
Clarity Transparent Volume LOW Viscosity high Fibrin clots Absent WBUS <200
• Gram’s stain No bacteria Yellow/ green yellow turbid Transparent
Visit www.dralamzeb.com for more knowledge and updates
TREATMENT:
1. Specific antibacterial.
Acute infectious arthritis should be treated as soon as possible with specific antibiotics particularly following sensitivity tests, in order to avoid irreversible changes in the joint. The antibiotics should administer for several days and even after clinical recovery. antibiotics used should be of lower molecular weight for belle 20,000 action into the synovial membrane. e.g. Penicillin- G (@ dose di
20,000 1.u. /kg) and Streptomycin (@ dose of 10-20 mg/kg) alone a combination, Terramycin, Kanamycin (® dose of 6 mg/kg), Gentamicin, a dose of 2 mg/kg), Oxacillin, Methicillin,
Cephalosporin,
Erythromycin, T’ylosin (for mycoplasmos1s).
- Analgesics as sodium salicylate, @ dose of 25-50 gm/LA, PO, or.
- phenylbutazone, @ dose of 2 gm/300 kg, PO, may be advised to reduce pain in acute stages of the disease.
- In chronic suppurative arthritis, joint lavage may be recommended.
- This is achieved by aspiration of exudate from the joint capsule by using a sterile syringe and needle followed by irrigation with solution of antibiotics in sterile normal saline at pfI 7.0. Surgical drainage, debridement of the membrane, and articular surface may sometimes be required for removal the necrosed structures.
- In chronic arthritis, intra-articular injection of antibiotics combined with proteolytic enzymes may be useful.
- In non suppurative arthritis, the use of long acting corticosteroid with antibiotics by IA route, to reduce local swellings and pain. For this purpose, Methylprednisolone acetate, @ dose of 20-40 mg/joint or Prednisolone, @ dose of 2-5 ml/joint are in common (in human medicine).
For more details and reference visit here