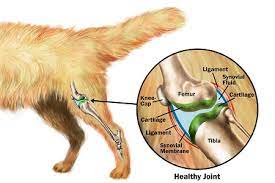
Arthropathy is also known as Degenerative joint disease, Arthrosis, Polyarthritis & Osteoarthrosis
Definition
It is a non-inflammatory disease of the joints
Which includes degenerative, erosive changes & lesions at articular cartilage, eburnation of sub-chondral bones, & hypertrophy of bone surrounding articular cartilage.
It is characterized clinically by
(1)- stiffness of the joint(s)
(2)- chronic progressive lameness.
Etiology:
- Primary arthropathy results from wear and tear as a part normal aging process. It may be due to inheritance may be a factor.
The etiology of secondary arthropathy:
I. Conformational or angular limb deformities caused by either congenital or acquired.
Ii. Acute and repeated traumatic injuries at the joint increase the rate of cartilage loss.
Iii. Nutritional deficiencies include calcium, phosphorus, copper, manganese, and magnesium. Examples include rickets osteodystrophy fibrosis (horse), and osteocalcin (ruminants).
Iv. Chronic chemical poisonings, such as zinc, fluorine, and selenium.
V. Metabolic disorders, hormonal imbalances, obesity, and inherited spasticity have also been reported to be the causes of arthropathy.
W
In primary arthropathy with increasing age, there is a loss of normal resilience of cartilage, because of the lowering of chondroitin sulfate and reduction in permeability of the cartilaginous matrix, which can result in progressive degeneration of articular cartilage.
Secondary arthropathy
This result in greater shearing stress on some particular points, causing erosions of the cartilage, and increasing the density of sub-
Chondral bone, and proliferation of bone and cartilage at articular margins. There may be no remarkable change in synovial fluid. Cartilage damage can also occur through the indirect pathways, i.e., Damage to chondrocytes and the release of lysosomal enzymes that may cause the loss of intercellular proteoglycans, thus more wearing off the cartilage.
Clinical Pathology
1)- Quality & quantity of synovial joint remains normal.
2)- Proliferative and degenerative changes.
3)- Imbalance of serum, Ca, and phosphorus levels.
Symptoms
(1)- Joint Pain
(2)- Joint Stiffness
(3)- Crepitus
(4)- Alteration in joint shape
(5)- Functional Impairment
Signs
1)- Restricted movement
2)- Limp
3)- Deformity
4)- Bony Swelling
5)- Soft tissue swelling
6)- Muscle atrophy/weakness
7)- Tenderness (joint line, periarticular)
Necropsy Findings
Joint cartilage becomes discolored, thin, patchily eroded, ulcerated & sometimes folded. The non-articular surface contains osteophyte deposits. Calcification of joint capsule & chip fracture of the head of the tibia. The head of the long bone becomes smaller than normal. The synovial lining becomes thick, red & proliferative.
Time Course
Slow Onset
Lifestyle measures
1)- Provide soft, flat, and dry floor
2)- Provide a balanced diet
3)- Ca, phosphorous & other minerals can delay the degeneration process. NB: In cases of irreversible, troublesome, multiple, and chronic joint lesions, slaughter or euthanasia should be considered.

Good post. I learn something new and challenging on blogs I stumbleupon on a daily basis. Its always exciting to read content from other authors and use a little something from other web sites.
Great info 👍🏻